
Role of miR-944/MMP10/AXL- axis in lymph node metastasis in tongue cancer.
Clinical collaborator:Dr. Rajendra Badwe (TMC) and Dr. Sudeep Gupta (TMC)
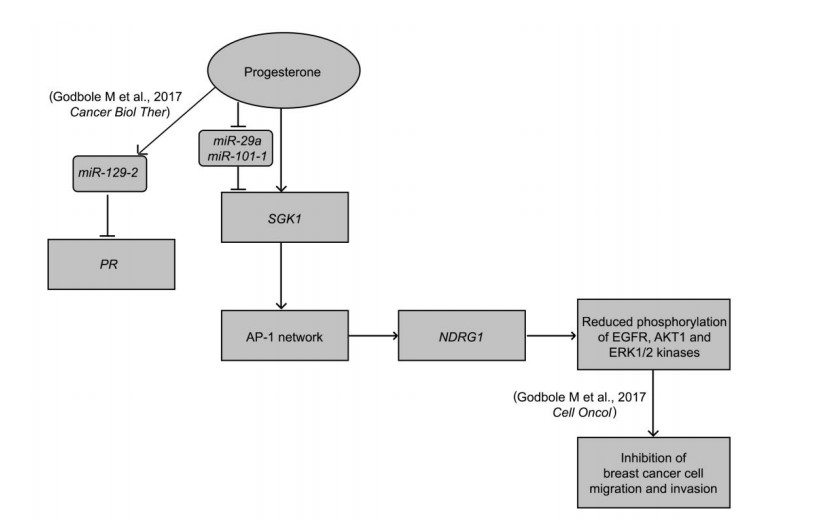
Operable breast cancer (OBC) surgery performed among premenopausal have a better outcome if carried out in the luteal rather than the proliferative phase of the menstrual cycle. In a randomized clinical trial on OBC patients, a single dose of progesterone-- the dominant hormone during luteal phase-- administered before surgery (preoperative) showed an increased period of disease-free survival in patients. Of several hypothesis-generating results from this trial, the survival benefit to breast cancer patients independent of their progesterone receptor (PR) status, raised an important question about how progesterone affects the outcome of PR-negative cells? We set out to specifically ask how progesterone affects the outcome of PR-negative cancer. We performed microarray and RNA-Seq-based gene expression profiling and ChIP-Seq analyses of breast cancer cells treated with progesterone to identify genomic targets of progesterone, followed by functional characterization of the target genes. We identify that progesterone acts through the down-regulation of its own receptor via increased expression of a microRNA miR-129-2, and through up-regulation of a novel signaling cascade independent of the PR status of breast cancer cells. In addition, progesterone up-regulates a SGK1/AP-1/NDRG1 axis, along with the down-regulation of miR-29a and miR-101-1 that regulates the expression of components of this cascade. We further establish that NDRG1, N-Myc downstream regulated gene 1, a tumor metastasis suppressor gene inactivates a set of kinases impeding the invasion and migration of breast cancer cells, providing a molecular basis to the phenotypic alterations induced by progesterone. Furthermore, our analysis suggests that inhibition of miR-129-2 could reinstate the expression of PR, which could help stabilize PR levels in the patients with PR-negative breast cancer.
Tongue cancer is a relatively common malignancy associated with severe disease and treatment-related morbidity. The presence of regional occult lymph node metastasis is one of the important factors for poor clinical outcomes. Lymph node metastasis is observed in 27-40% of early-stage tongue cancer patients. Presence of even a single cancer-positive lymph node leads to a poor 5-year survival of below 50%. To improve patient survival, it is necessary to understand the underlying mechanisms of metastasis. We previously reported over-expression of MMP10 (Oral Oncology 2017) in tongue tumors to be associated with nodal metastases in early-stage tongue cancer patients.
Here, we analyzed 219 early-stage tongue cancer resected specimens for MMP10 expression obtained from patients before surgery, including phase 3 trial N-zero clinical trial samples. We find upregulation of MMP10 in 86% of primary tongue tumors with lymph node metastases (p<0.0001). We show miR-944 negatively regulates MMP10 by targeting its 3'-UTR and overexpression of miR-944 or loss of MMP10 suppresses proliferation, migration and invasion of tongue cancer cells in vitro and impedes nodal metastasis in orthotopic tongue cancer mouse model. Importantly, overexpression of MMP10 induces tumor growth and nodal metastasis mediated through the AXL signaling pathway inducing epithelial mesenchymal transition (EMT) phenotype. Knockdown of AXL suppresses MMP10-mediated proliferation, migration and invasion of tongue cancer cells, indicating AXL to be a candidate therapeutic target in tongue cancer. To summarize, our study establish miR-944/MMP10/AXL- axis underlie lymph node metastases among early-stage tongue cancer patients. Additionally, low expression of miR-944 or overexpression of MMP10 as a prognostic biomarker could also help predict nodal metastasis in tongue cancer, an assessment that awaits designing a larger prospective randomized clinical trial.